In Minnesota, roughly 1 million people have health care coverage through Medicaid, also known as Medical Assistance (MA).1 Nationally, about 72 million people were enrolled as of October 2024.2 These include seniors, children, people living with disabilities, and people who work in jobs that don’t pay enough to make ends meet. Through Medicaid, people can afford essential health care services and supports.
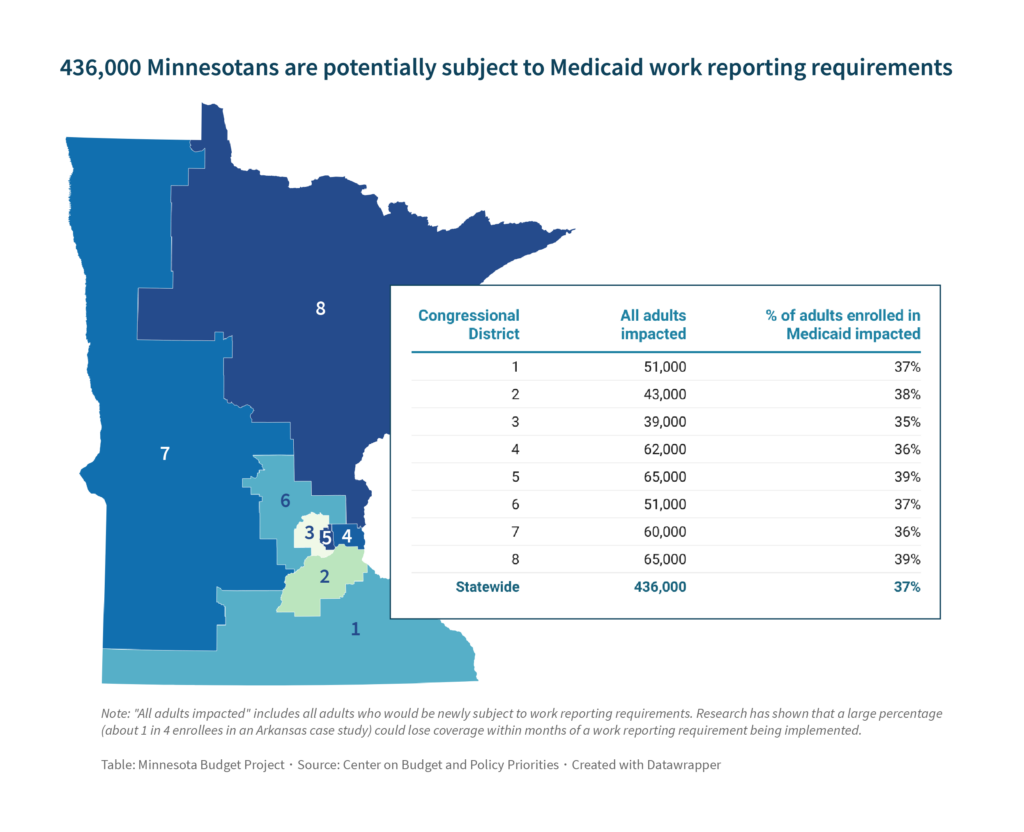
Medicaid is funded jointly by the federal government and the states. But recent budget proposals from federal Republicans show the federal government is considering stepping back from their commitments and introducing harmful significant cuts and changes to Medicaid. “Work reporting requirements” are one such proposal that could cut funding for Medicaid by $100 billion over the next 10 years.3 If enacted, these requirements would apply to 36 million people across the country, including 436,000 Minnesotans, and put their health care coverage at risk.4
Work reporting requirements would mean fewer people could afford the health care they need, would add unnecessary complexity and paperwork, increase costs for states, and would not increase employment.
Medicaid is a vital source of affordable health care coverage for people all across the state
Affordable and accessible health care is a vital part of healthy and thriving communities.5 The 60-year-old federal Medicaid program is the mechanism through which one out of every six adult Minnesotans under the age of 65 receive affordable health coverage.6 Medicaid is known as Medical Assistance, or MA, in Minnesota, and in 2023 included roughly 620,000 children, 120,000 people with disabilities or blindness, and 90,000 seniors.7 Minnesota is one of 41 states that adopted the federal option to cover lower-income individuals; this is sometimes called the “Medicaid expansion,” and the federal government covers a higher share of their cost of care.8
Most Medicaid participants who can work, do work, and those who do not work face substantial barriers to finding and keeping a job. In Minnesota, 70 percent of adults covered by Medicaid are employed.9 And this follows the national trend: almost two-thirds of Medicaid enrollees aged 19 to 64 work. Most of the remaining individuals have a disability, are caring for family members, or attend school.10
Work reporting requirements threaten health coverage for hundreds of thousands of Minnesotans
Medicaid is an essential pathway to affordable health care for people across the state, and work reporting requirements would put many at risk of losing their coverage. Work reporting requirements are policies that require certain enrollees to submit documentation to prove that they have worked a certain number of hours over a period of time, as a condition to receive Medicaid coverage.11
Analysis by the Center on Budget and Policy Priorities estimates that roughly 436,000 Minnesotans — 37 percent of all adults covered by Medicaid — could be subject to work reporting requirements that puts their health coverage at risk.12 Nationally, health care coverage for 36 million people would depend on their ability to meet work reporting requirements — that’s 44 percent of all Medicaid enrollees in the U.S. This analysis assumes those aged 19 to 64 years old who are not enrolled through disability pathways would be subject to work requirements. Those losing health care coverage would include people who do not secure the required number of work hours, but also people who do meet the work requirements but are unable to successfully navigate complicated reporting timelines, arduous paperwork, and a likely lack of capacity at the state level to get answers to questions they may have.
Even if they are exempted from having to meet work reporting requirements, people who are full-time caretakers or have disabilities or illnesses that keep them from paid work could still lose their health coverage because of challenges meeting paperwork requirements. Work reporting requirements would also lead to coverage loss for people who are working. For example, someone could lose their coverage because they failed to return a required form, or because their paperwork was lost in the mail. The unnecessary reporting requirements add a burden for people that could cause them to lose coverage because of a simple paperwork mistake. Loss of health care can also occur for people who are in between jobs.13
Work reporting requirements harm some groups more than others
While the specifics of who would be harmed depend on the specifics of any work reporting proposal, research has shown that some groups are more likely to lose their health care coverage than others. These are people who are already marginalized due to historic and current barriers to economic opportunities. The loss of health coverage would likely disproportionally affect people with disabilities, women, people experiencing homelessness, and people with mental health conditions or substance use disorders.14 Other groups likely to be harmed by reporting requirements are people living in rural areas or with transportation barriers, facing language or literacy barriers, in poor health, have limited mobility, or have limited internet access. These limitations can make the process of reporting their work and returning paperwork even more difficult, which would likely lead to a higher loss of health care coverage.
Prior attempts at work reporting requirements have been costly and led to large losses of health coverage
Work reporting requirements have been attempted in several states. They led to substantial loss of health care coverage, high costs for states, and widespread confusion and frustrations, as seen in the three case studies below.
- In Arkansas, about 1 in 4 enrollees subject to the reporting requirements lost coverage in only seven months in 2018 before a federal court halted the program.15 A large share of the people who lost coverage were likely still eligible for Medicaid but did not reapply.16 The work reporting requirements were stopped by a federal judge in early 2019.
- In 2019, New Hampshire implemented work reporting requirements that had more flexibility and more community outreach than in Arkansas. Even still, the New Hampshire Department of Health and Human Services had trouble reaching enrollees, and among enrollees who were reporting work hours, many were not meeting the required amount. Two-thirds of people subject to requirements were poised to be disenrolled after just two months. Before the mass disenrollments could occur, New Hampshire suspended the program and a federal court halted it altogether.17
- Georgia includes work reporting requirements that apply to a specific new group of applicants with low incomes. The cost of implementing the requirements was initially estimated to be roughly $2,490 per person. At the end of the first year, it ended up costing about $13,360 per enrollee. Only about one-third of that spending was on health care; the rest went to systems modifications to implement the program and other administrative expenses.18
These examples demonstrate how folks lose their coverage due to work reporting requirements, including many who likely would still qualify for coverage. They also show how burdensome work reporting requirements are to both Medicaid participants and the state governments that enact them. States often fail to hire enough staff to respond to people’s questions or to manage the process for work reporting and screening for exemptions.19
Work reporting requirements are not effective in increasing employment
Proponents of work reporting requirements often say their goal is incentivizing people to work.20 But research has shown that they do not increase employment. The federal Congressional Budget Office concluded that a 2023 federal House bill to implement Medicaid work reporting requirements would lead to health coverage loss with no change in employment or hours worked.21 This was true in Arkansas where work reporting requirements were implemented. Following up over 18 months showed they did not increase employment.22 Further, studies on work reporting requirements in SNAP have shown that work reporting requirements have no effects on employment.23
In fact, the main barriers to work for low-income adults are economic conditions outside their control.24 Strict rules that require people to consistently work a set number of hours every week or every month do not match the reality of low-wage work. Lower-income adults are especially at risk of unexpected changes in hours worked as well as job market fluctuations. When unemployment rates are low, people tend to work more hours. But when unemployment rates are high, folks working in low-wage jobs are more often the first to lose their jobs and see drops in their hours at work. Low-income workers are also more likely to have unpredictable and fluctuating work hours in general, even if they are employed in multiple positions. These employment fluctuations could lead to gaps or loss of health coverage if Medicaid work reporting requirements are in place. Work reporting requirements do not take into account that some people live in places with few job opportunities. They simply make life and good health harder for low-income people by erecting barriers to getting health care.
Policymakers should reject work reporting requirements
For many in Minnesota and across the nation, Medicaid is synonymous with health. It means that when working people get sick, they can get the care they need to recover and get back on the job. It means a mother is able to afford medication for a child, a student receives mental health supports, and an older adult is able to live safely in their home. Proposed federal work reporting requirements endanger access to affordable health care coverage for 436,000 Minnesota adults. Policymakers at both the federal and state levels should reject work reporting requirements and cuts to Medicaid in any other form, so we can continue to embrace our values as a state where all of us, regardless of race or place or ability, are able to survive and thrive.
By Jessie Luévano
[1] Enrollment as of January 2025. Minnesota Department of Human Services, Managed care enrollment figures, February 2025.
[2] KFF, Medicaid and Chip Monthly Enrollment, October 2024.
[3] Politico, House GOP puts Medicaid, ACA, climate measures on chopping block, January 2025.
[4] Center on Budget and Policy Priorities, Medicaid Work Requirements Could Put 36 Million People at Risk of Losing Health Coverage, February 2025.
[5] U.S. Department of Health and Human Services, Health Care Access and Quality, accessed February 2025.
[6] Adults in this case refer to people aged 19 to 64. KFF, Medicaid in Minnesota, August 2024.
[7] Minnesota Department of Human Services, Who Medicaid and MinnesotaCare serve, 2023.
[8] KFF, Status of State Medicaid Expansion Decisions, November 2024.
[9] KFF, Medicaid in Minnesota, August 2024.
[10] In this analysis, “work” is defined as being employed either full time or part time. Center on Budget and Policy Priorities, Research Note: Most Medicaid Enrollees Work, Refuting Proposals to Condition Medicaid on Unnecessary Work Requirements, November 2024.
[11] Economic Policy Institute, Work requirements for safety net programs like SNAP and Medicaid, January 2025.
[12] Center on Budget and Policy Priorities, Medicaid Work Requirements Could Put 36 Million People at Risk of Losing Health Coverage, February 2025.
[13] The Center for Law and Social Policy, The Racist Roots of Work Requirements in Public Benefits Programs, January 2025.
[14] Center on Budget and Policy Priorities, Medicaid Work Requirements Could Put 36 Million People at Risk of Losing Health Coverage, February 2025.
[15] Center on Budget and Policy Priorities, Pain But No Gain: Arkansas’ Failed Medicaid Work-Reporting Requirements Should Not Be a Model, August 2023.
[16] Center on Budget and Policy Priorities, Medicaid Work Requirements Could Put 36 Million People at Risk of Losing Health Coverage, February 2025.
[17] Urban Institute, New Hampshire’s Experience with Medicaid Work Requirements, February 2020.
[18] Center on Budget and Policy Priorities, Georgia’s Medicaid Experiment Is the Latest to Show Work Requirements Restrict Health Care Access, December 2024.
[19] Center on Budget and Policy Priorities, Medicaid Work Requirements Could Put 36 Million People at Risk of Losing Health Coverage, February 2025.
[20] Economic Policy Institute, Work requirements for safety net programs like SNAP and Medicaid, January 2025.
[21] Congressional Budget Office, CBO’s Estimate of the Budgetary Effects of Medicaid Work Requirements Under H.R. 2811, the Limit, Save, Grow Act of 2023, April 2023.
[22] Health Affairs, Medicaid Work Requirements In Arkansas: Two-Year Impacts On Coverage, Employment, And Affordability Of Care, September 2020.
[23] American Economic Journal: Economic Policy, Employed in a SNAP? The Impact of Work Requirements on Program Participation and Labor Supply, February 2023.
[24] Economic Policy Institute, Work requirements for safety net programs like SNAP and Medicaid, January 2025.